Addressing unmet challenges in CAR T cell therapeutics
CAR T cell therapies have revolutionized the treatment of hematological malignancies such as leukemia and lymphoma, however the manufacturing process is extremely costly and slow due to its bespoke nature. Allogeneic CAR-T cell therapy, using cells from healthy donors, provides an essential alternative which could lead to ‘off-the-shelf’ solutions instead. Induced pluripotent stem cells (iPSCs) provide a standardized and scalable approach. Evotec's recent study showcases iPSC-derived T cells targeting cancer cells with precision, hinting at a promising future toward accessible and standardized cancer immunotherapies.
Cell-based therapy, which involves the use of living cells to combat diseases, has recently seen remarkable growth, both in clinical applications and within the pharmaceutical industry. As a result, it is now considered one of the most promising therapeutic approaches for cancers.
In particular, chimeric antigen receptor (CAR) T cell therapy has demonstrated significant clinical success in recent years, particularly in the treatment of hematological malignancies. Several CAR-T therapies have received approval from regulatory bodies such as the Food and Drug Administration (FDA) and the European Medicines Agency (EMA), providing critical treatment for various hematological cancers [1].
However, autologous CAR-T cell therapy, which uses T cells isolated from the patient’s peripheral blood, is often slow, complex, and costly due to its bespoke nature [2]. Furthermore, manufacturing success is often dependent upon the availability and condition of the initial autologous T cells. Patients may have undergone prior treatments that compromise the quality and quantity of their immune cells, further complicating the production process and reducing the likelihood of success.
To overcome these challenges, researchers are exploring the use of allogeneic T cells sourced from healthy donors, aiming to create "off-the-shelf" therapies readily available for patients. This approach could streamline the production process and potentially allow for multiple modifications to target different tumor antigens, enhancing efficacy and accessibility.
While this approach represents a promising avenue for streamlining and standardizing T cell therapy, there are still inevitable drawbacks with the manufacturing process. Allogeneic T cells need to be extensively genetically modified to prevent alloreactivity and immunogenicity, as well as ensuring tumor-specific activity. However, engineering T cells presents significant challenges, including reduced production yield; genotoxicity due to off-target effects; and the development of an exhausted T cell phenotype and product owing to the need for prolonged ex vivo expansion [3].
Induced pluripotent stem cells (iPSCs) offer an alternative approach. iPSCs provide a standardized, scalable cell source that can be precisely engineered for therapeutic use [3]. These cells are easier to genetically engineer and have a much higher proliferative capacity, ensuring a stable and plentiful cell source. By establishing master cell banks of iPSCs, researchers can ensure consistent quality and quantity of starting materials, reducing variability across CAR-T or T-cell receptor (TCR)-T products and creating more accessible, standardized, and effective treatments for cancer patients. In this article, we will highlight a promising iPSC approach for targeting tumor cells, providing a pathway towards scalable and GMP-compliant off-the-shelf cancer therapies.
Developing off-the-shelf T cell therapies
iPSCs provide a crucial off-the-shelf source of therapeutic T cells, offering significant advantages in scalability and genetic engineering capabilities. By leveraging iPSC technology, researchers can generate T cells with the potential for infinite expansion and tailor them to possess specific therapeutic functions through straightforward genetic manipulation.
Importantly, genetic engineering of iPSCs enables the generation of fully modified clonal lines, facilitating rigorous safety assessments and ensuring consistent therapeutic outcomes. However, realizing the full potential of iPSC-derived T cell therapy is dependent on the development of a robust and scalable production process that meets Good Manufacturing Practice (GMP) standards. Moreover, it's essential that this process yields mature T cells expressing the TCRα and TCRβ isoforms, commonly known as αβ T cells, which constitute the majority of T cells.
However, current manufacturing methods often suffer from low differentiation efficiency and poor scalability, hindering widespread application [4]. This is partially due to the complex differentiation processes that are required to generate T cells from iPSCs. Standard T cell differentiation protocols rely on different types of murine feeder cells to support prolonged in vitro proliferation. These murine feeders are unable to divide and provide essential extracellular secretions for iPSC proliferation, hematopoietic progenitor induction, and T cell differentiation. However, each feeder requires different sets of serum and basal media for maintenance culture and co-culture with differentiating iPSCs, complicating safety, control, and reproducibility. As such, a significant part of developing “off the shelf” T cell therapies is the establishment of a feeder-free culture for all stages of iPSC differentiation.
Modified iPSC lines successfully target cancer cells
In a recent study, researchers from Evotec examined the production of CD8+ T cells using Evotec's fully scalable, GMP-compliant iPSC-derived αβT (iαβT) cell differentiation process. The researchers used a validated GMP iPSC line, which had been modified with a NY-ESO-1 specific TCR knock-in. This TCR targets NY-ESO-1, a cancer-germline antigen that is expressed in a wide range of tumor types.
Using this cell-line, the researchers established a feeder-free differentiation protocol to efficiently generate iαβT cells. Each stage of the process was rigorously monitored using flow cytometry and single-cell transcriptome analysis. From iPSCs enriched with the knock-in modification, hematopoietic progenitor cells (HPCs) were induced and differentiated into iαβT cells (Figure 1). Throughout differentiation, cells displayed T cell markers CD45, CD5, and CD7, and initiated NY-ESO-1-specific TCR expression.
Following activation of T cell differentiation by Notch signaling, the proportion of NY-ESO-1-TCR positive cells surged to over 95%. Transcriptome analysis confirmed the successful differentiation from pluripotent cells to those with a T cell-specific gene expression profile.
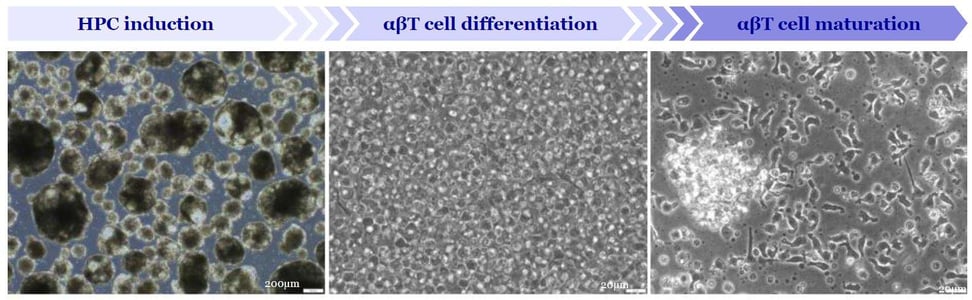
Figure 1: Morphology of cells during differentiation process. Evotec has developed a 3D scalable, feeder-free induction process of Hematopoietic Progenitor Cells (HPCs). After enrichment of CD34-positive cells, T cell differentiation is initiated by activation of Notch signaling in a feeder-free process that will be further developed based on Evotec’s know-how with other immune cell types.
Importantly, the iαβT cells were shown to express CD8α and CD8β, which are both crucial for cytotoxic T cell function. Co-culture experiments with NY-ESO-1 antigen presenting tumor cell lines confirmed the cytotoxic activity of iαβT cells and their ability to release cytokines such as TNF-α and IFN-γ (Figure 2).
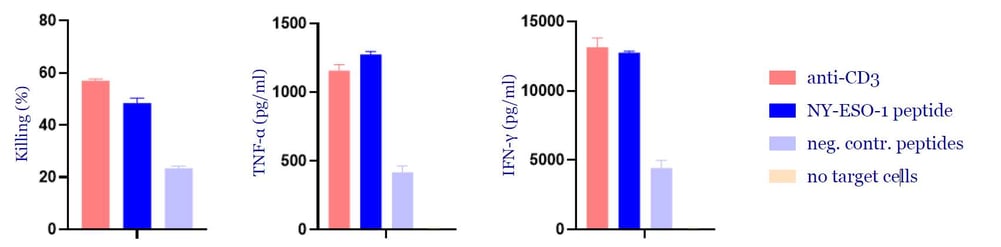
Figure 2: Functional characterization of iαβT cell. iαβT cells were cocultured with a tumor cell line loaded with the NY-ESO-1 peptide or negative control peptides. Anti-CD3 antibodies were used as a positive control. Cytotoxic activity and the release of cytokines (TNF-α and IFN-γ) was analyzed.
These results demonstrate that the Evotec iαβT differentiation process can efficiently generate CD8+ T cells that secrete cytokines and show cytotoxic activity, indicating their potential as a promising cell source for TCR-T or CAR-T cancer immunotherapies.
Evotec’s in-house GMP production pipeline
Evotec has built an iPSC infrastructure that represents one of the largest and most sophisticated platforms in the industry. Its growing portfolio includes natural killer cells (iNK), macrophages (iMACs) and αβ and γδ T cells (iT) (Figure 3). Each type of immune cell can serve as a foundation for creating numerous differentiated allogeneic cell therapy products.
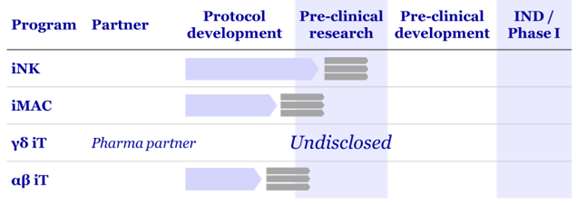
Figure 3: Evotec’s iPSC-based cell therapy pipeline for oncology
Evotec’s iPSC platform is closely connected to a variety of in-house key technologies, which - together with a strong focus on standardization, upscaling and quality control (QC) – enable the efficient generation, characterization, and differentiation of iPSCs. . Supported by Evotec’s world class GMP manufacturing facilities, novel allogeneic cell therapeutics can be developed without the complexities or production bottlenecks associated with autologous therapies.
Starting with genetically engineered iPSC GMP master cell banks, Evotec’s cell therapeutics manufacturing platform provides a fully integrated pipeline encompassing all stages from research to development and manufacturing of cell therapy products. From the initial project inception to clinical application, Evotec excels in efficiently producing a diverse array of "off-the-shelf" cell therapy products (Figure 4)

Figure 4: Schematic depiction of Evotec’s fully scalable GMP manufacturing process.
From tailor-made to off-the-shelf solutions
Allogeneic T cell platforms are driving the transition from customized to standardized T cell therapy, addressing the urgent need of patients both in cell quality, consistency, and delivery time. However, realizing the full potential of iPSC-derived T cell therapies requires the development of scalable and GMP-compliant production pipelines.
By producing a feeder-free culture for all stages of PSC differentiation, Evotec provides an efficient, reproducible, and scalable way to produce iPSC-derived αβT cells that can effectively target tumors. Thanks to Evotec’s expansive iPSC differentiation platform, iPSCs are one step closer to producing essential T cell-based cancer immunotherapies for the future.
Find out more about Evotec’s industry leading cell therapy platform
References
- Chen, Y.J., Abila, B., & Mostafa Kamel, Y. (2023). CAR-T: What Is Next? Cancers, 15(3), 663. https://doi.org/10.3390/cancers15030663
- Gajra, A., Zalenski, A., Sannareddy, A., Jeune-Smith, Y., Kapinos, K., & Kansagra, A. (2022). Barriers to Chimeric Antigen Receptor T-Cell (CAR-T) Therapies in Clinical Practice. Pharmaceutical Medicine, 36(3), 163–171. https://doi.org/10.1007/s40290-022-00428-w
- Netsrithong, R., Garcia-Perez, L., & Themeli, M. (2024). Engineered T cells from induced pluripotent stem cells: From research towards clinical implementation. Frontiers in Immunology, 14. https://doi.org/10.3389/fimmu.2023.1325209
- Iriguchi, S., Yasui, Y., Kawai, Y., Arima, S., Kunitomo, M., Sato, T., et al. (2021). A clinically applicable and scalable method to regenerate T-cells from iPSCs for off-the-shelf T-cell immunotherapy. Nature Communications, 12(1), 430. https://doi.org/10.1038/s41467-020-20658-3
