Stem cells are undifferentiated or partially differentiated cells that can proliferate indefinitely and give rise to various types of specialised cells. They are, therefore, very interesting for therapeutic purposes. In 2006, Shinya Yamanaka’s lab in Japan demonstrated that the introduction of four specific transcription factor genes, now known as Yamanaka factors, could convert differentiated, somatic cells into pluripotent stem cells (also known as iPS cells or iPSCs). For this discovery, Yamanaka was awarded the 2012 Nobel Prize along with Sir John Gurdon, honouring their findings that mature cells can be reprogrammed to become pluripotent.
The iPSC technology holds great promise in the field of regenerative medicine. iPSCs represent an invaluable source of cells, e.g. to replace lost, damaged or diseased cells. Specifically, iPSCs have significant potential in disease areas with high unmet medical need, e.g. neurodegenerative diseases such as Alzheimer’s, ALS or Huntington’s or conditions such as diabetes or age-related macular degeneration (AMD). In these indications, the application of iPSC-based models represents a paradigm shift in developing desperately needed new therapies.
Why iPSCs?
Compared to previous models, patient-derived iPSCs are more physiologically relevant and better suited for modelling disease pathophysiology and for understanding a drug’s mechanism of action. Therefore, iPSC-based high-throughput screening approaches provide unique opportunities as a tool for disease modelling and predicting drug efficacy. This is especially important in complex, age-related or genetic indications such as neuronal diseases. Moreover, patient-derived iPSCs may eventually be utilised to stratify patient populations for clinical trials - a key success factor for electing better and safer drugs for clinical development in disease areas with high unmet clinical need.
iPSCs at Evotec
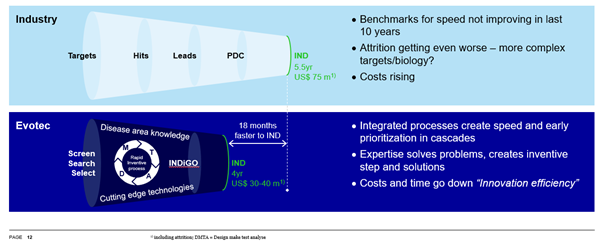
Evotec has built one of the largest and most sophisticated iPSC platforms in the industry. The platform has been developed over recent years with the goal to industrialise iPSC-based drug screening in terms of throughput, reproducibility and robustness to reach the highest industrial standards, and to use iPSC-based cells in cell therapy approaches via the Company’s proprietary EVOcells platform.
While culturing and differentiating iPSC-derived cells in a reproducible manner at industry scale used to be a challenge in the past, Evotec has succeeded in establishing scalable and robust protocols that allow a stable production of specific disease-relevant cell types. This includes generation of a cell bank of fully validated iPSC lines, upscaling of iPSC culture and differentiation protocols to industry standards, as well as automation of iPSC-derived cultures - all meeting the highest quality control standards.
In addition to phenotypic screening, Evotec has developed more complex models, such as co-cultures of multiple cell types or microfluidic organs-on-a-chip approaches, which enable interaction between different cell types. These systems allow the modelling of human diseases under conditions that closely resemble the physiological environment.
Smart Partnerships
Evotec has entered into several long-term partnerships that leverage the Company’s iPSC platform to develop highly relevant disease models, e.g. with Bristol Myers Squibb (formerly Celgene) in neurodegeneration (2016), and with Centogene in rare diseases (2018).
In its TargetRD project in collaboration with Centre for Regenerative Therapies TU Dresden, Evotec is using the advances in iPSC technology to generate iPSC-derived Retinal Pigment Epithelium cells from patients with retinal degenerative diseases to accelerate drug discovery.
Read our DDup on iPSC-Based Drug Discovery
Read our DDup focused on iPSC-Based Drug Discovery and Retinal Disease